IMAGE: https://www.unaids.org/en/resources/presscentre/featurestories/2020/may/20200525_modelling-the-extreme
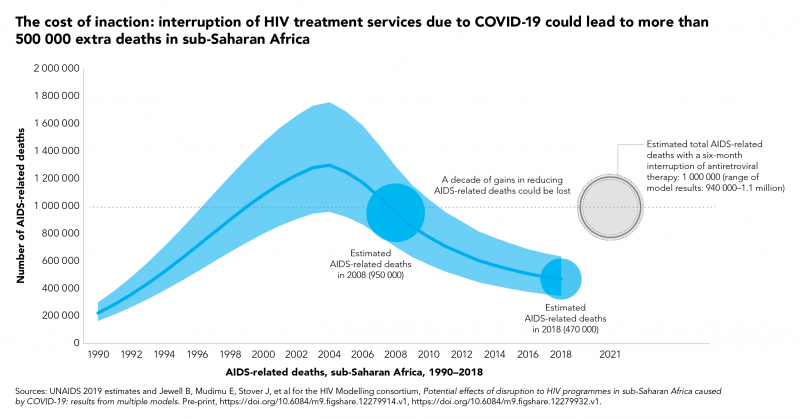
The World Health Organization warns that a six-month disruption of antiretroviral therapy could lead to more than 500 000 extra deaths from AIDS-related illnesses, including from tuberculosis, in sub-Saharan Africa in 2020–2021.
The cost of inaction: COVID-19-related service disruptions could cause hundreds of thousands of extra deaths from HIV (source):
Gains made in preventing mother-to-child transmission of HIV could be reversed, with new HIV infections among children up by as much as 104%
A modelling group convened by the World Health Organization and UNAIDS has estimated that if efforts are not made to mitigate and overcome interruptions in health services and supplies during the COVID-19 pandemic, a six-month disruption of antiretroviral therapy could lead to more than 500 000 extra deaths from AIDS-related illnesses, including from tuberculosis, in sub-Saharan Africa in 2020–2021. In 2018, an estimated 470 000 people died of AIDS-related deaths in the region.
There are many different reasons that could cause services to be interrupted—this modelling exercise makes it clear that communities and partners need to take action now as the impact of a six-month disruption of antiretroviral therapy could effectively set the clock on AIDS-related deaths back to 2008, when more than 950 000 AIDS-related deaths were observed in the region. And people would continue to die from the disruption in large numbers for at least another five years, with an annual average excess in deaths of 40% over the next half a decade. In addition, HIV service disruptions could also have some impact on HIV incidence in the next year.
“The terrible prospect of half a million more people in Africa dying of AIDS-related illnesses is like stepping back into history,” said Dr Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization.
“We must read this as a wake-up call to countries to identify ways to sustain all vital health services. For HIV, some countries are already taking important steps, for example ensuring that people can collect bulk packs of treatment, and other essential commodities, including self-testing kits, from drop-off points, which relieves pressure on health services and the health workforce. We must also ensure that global supplies of tests and treatments continue to flow to the countries that need them,” added Dr Tedros.
In sub-Saharan Africa, an estimated 25.7 million people were living with HIV and 16.4 million (64%) were taking antiretroviral therapy in 2018. Those people now risk having their treatment interrupted because HIV services are closed or are unable to supply antiretroviral therapy because of disruptions to the supply chain or because services simply become overwhelmed due to competing needs to support the COVID-19 response.
“The COVID-19 pandemic must not be an excuse to divert investment from HIV,” said Winnie Byanyima, Executive Director of UNAIDS. “There is a risk that the hard-earned gains of the AIDS response will be sacrificed to the fight against COVID-19, but the right to health means that no one disease should be fought at the expense of the other.”
When treatment is adhered to, a person’s HIV viral load drops to an undetectable level, keeping that person healthy and preventing onward transmission of the virus. When a person is unable to take antiretroviral therapy regularly, the viral load increases, impacting the person’s health, which can ultimately lead to death. Even relatively short-term interruptions to treatment can have a significant negative impact on a person’s health and potential to transmit HIV.
This research brought together five teams of modellers using different mathematical models to analyse the effects of various possible disruptions to HIV testing, prevention and treatment services caused by COVID-19.
Each model looked at the potential impact of treatment disruptions of three months or six months on AIDS mortality and HIV incidence in sub-Saharan Africa. In the six-month disruption scenario, estimates of excess AIDS-related deaths in one year ranged from 471 000 to 673 000, making it inevitable that the world will miss the global 2020 target of fewer than 500 000 AIDS-related deaths worldwide.
Shorter disruptions of three months would see a reduced but still significant impact on HIV deaths. More sporadic interruptions of antiretroviral therapy supply would lead to sporadic adherence to treatment, leading to the spread of HIV drug resistance, with long-term consequences for future treatment success in the region.
Disrupted services could also reverse gains made in preventing mother-to-child transmission of HIV. Since 2010, new HIV infections among children in sub-Saharan Africa have declined by 43%, from 250 000 in 2010 to 140 000 in 2018, owing to the high coverage of HIV services for mothers and their children in the region. Curtailment of these services by COVID-19 for six months could see new child HIV infections rise drastically, by as much as 37% in Mozambique, 78% in Malawi, 78% in Zimbabwe and 104% in Uganda.
Other significant effects of the COVID-19 pandemic on the AIDS response in sub-Saharan Africa that could lead to additional mortality include reduced quality clinical care owing to health facilities becoming overstretched and a suspension of viral load testing, reduced adherence counselling and drug regimen switches. Each model also considered the extent to which a disruption to prevention services, including suspension of voluntary medical male circumcision, interruption of condom availability and suspension of HIV testing, would impact HIV incidence in the region.
The research highlights the need for urgent efforts to ensure the continuity of HIV prevention and treatment services in order to avert excess HIV-related deaths and to prevent increases in HIV incidence during the COVID-19 pandemic. It will be important for countries to prioritize shoring up supply chains and ensuring that people already on treatment are able to stay on treatment, including by adopting or reinforcing policies such as multimonth dispensing of antiretroviral therapy in order to reduce requirements to access health-care facilities for routine maintenance, reducing the burden on overwhelmed health-care systems.
“Every death is a tragedy,” added Ms Byanyima. “We cannot sit by and allow hundreds of thousands of people, many of them young, to die needless deaths. I urge governments to ensure that every man, women and child living with HIV gets regular supplies of antiretroviral therapy—something that’s literally a life-saver.”
Sources:
Jewell B, Mudimu E, Stover J, et al for the HIV Modelling consortium, Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: results from multiple models. Pre-print, https://doi.org/10.6084/m9.figshare.12279914.v1, https://doi.org/10.6084/m9.figshare.12279932.v1.
Alexandra B. Hogan, Britta Jewell, Ellie Sherrard-Smith et al. The potential impact of the COVID-19 epidemic on HIV, TB and malaria in low- and middle-income countries. Imperial College London (01-05-2020). doi: https://doi.org/10.25561/78670.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
WHO
The World Health Organization provides global leadership in public health within the United Nations system. Founded in 1948, WHO works with 194 Member States, across six regions and from more than 150 offices, to promote health, keep the world safe and serve the vulnerable. Our goal for 2019-2023 is to ensure that a billion more people have universal health coverage, to protect a billion more people from health emergencies, and provide a further billion people with better health and wellbeing.





Fock UN. Too infested with Deep State and liberal farting for too high salaries.
Monkeys attack lab technician, STEAL Covid-19 blood samples in India
In the attached official document, dated 28. february 2020 the Danish ministry of health confirms that COVID-19 is NOT dangerous enough to comes on the “Almen farlig sygdom” (Dangerous illness) list, COVID-19 is NOT malignant and COVID-19 CANNOT be considered as very infectious.
I contacted the Danish ministry of health to have the document and contents confirmed, and they confirmed that everything is correct and that the document is a geniuen offcial document from the Danish ministry of health https://uploads.disquscdn.com/images/cb309992d1881142207e2e995f4e04080451aaba15f55c62c401879db1a46584.jpg
Yep, I heard in a programme that the average age of covid deaths is 81. A dangerous disease would be killing young people in the thousands.
Correct, the majority of death from COVID-19 is from already terminal patients.
And remember that there is a massive different between dying WITH COVID-19 and dying DUE to COVID-19.
But the average partyslave dont care about that, they just obey and worship whatever carbage is on the screens that day.
The deathrate of COVID-19 is something like 0.5 on a bad day.
COVID-19 is nothing else but a plandemic used to introduce and enforce evens stricter laws and convince everyone that dictatorship is the way to go; that way the party can take care of you even better and 24/7, even without you knowing it.
How nice of them…..
And if you read the book “The Invisible Rainbow” by Arthur Firstenberg ISBN 978-1-64502-009-7, then you get a very different view on all those “pandemics”.
Another hoax of the WHO political organisation aka the Chinese Health Organisation…